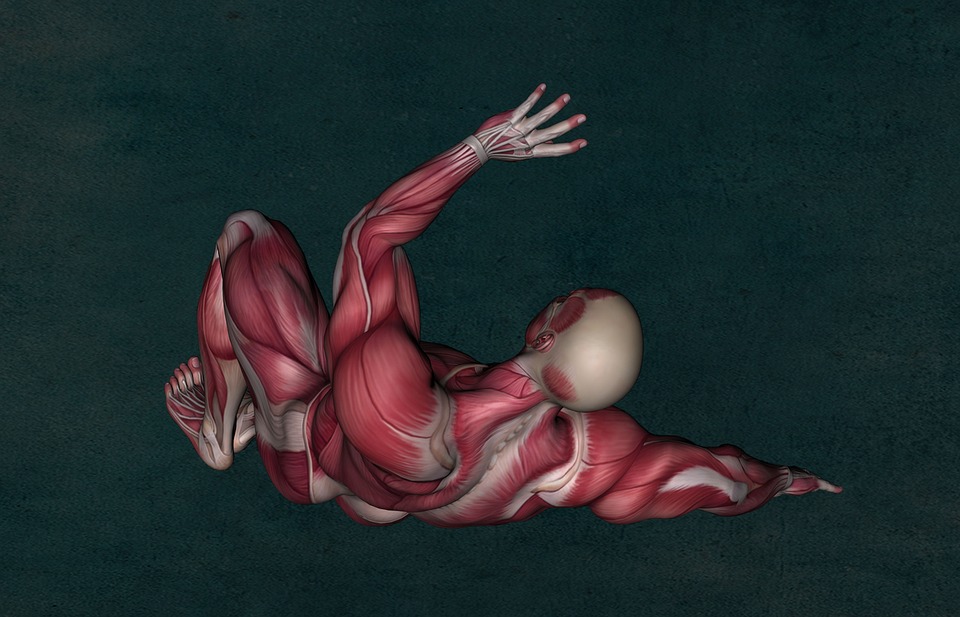
“Tendonitis”. Common words that are used for all types of pain in joints, from the ankle, all the way up to the wrist, elbow and shoulder. But what does it mean? Tendinopathies are altered healing responses of the tendon, which, when we analyze this tendon, show features that include alterations in the cells that make up the tendon. In many cases, the main driver of these conditions is altered mechanics at the joint, or above/below the joint, leading to increases in force and overuse of the tendon itself. With daily life, strength training, and athletic activity, there is a certain amount of “stiffness” that develops in the tendon, allowing it to deal with the demands of the activities presented to it. With tendinopathy, this stiffness is reduced, making the tendon less able to manage forces travelling through it. A quite complex topic, but there are certain take-home tips that may help you on your way to addressing this nagging pathology.
1. Genetics
Genetics can predispose you to tendinopathy, through Benign Connective Tissue Disorders, or other connective tissue diseases like Ehlers-Danlos. Your therapist may check your “Beighton Score” which will allow them to understand whether or not you are dealing with benign hypermobility that could be putting you at an increased risk3.
2. Co-Morbidities
Co-Morbidities can increase your risk of tendon disorders, as well as affect healing times from these disorders. Some of these co-morbidities may include diabetes, thyroid disorders (high or low), and kidney disease to name a few3.
3. Load
The load is one of the most important factors in tendon healing. As noted above, with this condition, the pathological structure of the tendon has changed. One must properly increase the tensile strength of the tendon, and in turn, affect the ground substance and cellular make up so that this tendon can better accommodate forces that are travelling through it. This will ultimately decrease the output that brought you into a clinic in the first place – pain. How long does this process take? Alfredson’s Achilles protocol, which has ample amounts of supporting evidence, shows that a 12-week program with 3 sets of 15 reps done 2x/daily, 7 days/week yielded best results. So the short answer – months.
4. Pain
Pain is an emotional experience unique to each individual, and as such, is acceptable to a certain extent during exercises, yet should not exceed 3-5/10 on the Visual Analog Scale during these exercises. Pain is often protective, so you are allowed to push through. However, the pain should return to baseline within 12-24 hours after having completed the set of exercises. If this is not the case, you should work with your physiotherapist to make adjustments where necessary4.
5. Eccentrics
Eccentrics are the eventual goal of the rehabilitation program, which is strengthening by gradually lengthening the tendon under load. That being said, to move straight to this type of contraction would be unwise. In most scenarios, the tendon is often briefly unloaded while other upper/lower body asymmetries are addressed. A primary progression to isometrics, which load the tendon without dynamic movement, should help further reduce pain/irritability, allowing the ultimate progression to dynamic eccentric loading to be a smooth process. Eventual progression to sport-specific movement would also be of benefit in most scenarios2.
Stay Mobile,
Travis Gaudet MScPT., BScKin., F.C.A.M.P.T., Dip.Manip.PT., cGIMS
References:
“Achilles Tendinopathy.” Manual Therapy, Churchill Livingstone, 2 Oct. 2002, www.sciencedirect.com/science/article/abs/pii/S1356689X02904583.
Alfredson, Håkan, and J Cook. “A Treatment Algorithm for Managing Achilles Tendinopathy: New Treatment Options.” British Journal of Sports Medicine, British Association of Sport and Excercise Medicine, 1 Apr. 2007, bjsm.bmj.com/content/41/4/211.short.
Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006 Feb 20;45(5):508-21.
Rio, Ebonie, et al. “The Pain of Tendinopathy: Physiological or Pathophysiological?” Sports Medicine (Auckland, N.Z.), U.S. National Library of Medicine, Jan. 2014, www.ncbi.nlm.nih.gov/pubmed/24027089.